صياغة التميز في البرمجيات
دعنا نبني شيئاً استثنائياً معاً.
اعتمد على شركة Lasting Dynamics للحصول على جودة برمجيات لا مثيل لها.
لويس لامبرت
ديسمبر 03, 2025 • 10 min read

In 2025, healthcare is witnessing a technological leap that is transforming every step of the care journey. الذكاء الاصطناعي, once confined mostly to administrative support and basic imaging, now includes generative models that assist with disease diagnosis, imaging enhancement, and decision support tools. According to Philips’ Future Health Index 2025, AI is moving from pilot projects into clinical workflows, helping with diagnostics, imaging, and administrative automation, but is worth mentioning that some clinicians and patients show a notable trust gap that limits broader deployment at the moment.
That said, the impact is already real: hospitals are using AI to streamline diagnostics, reduce reporting times, and aid clinicians in interpreting complex medical images. Virtual medical assistants are helping manage patient queries, triage, and follow-ups. Generative AI tools are being piloted in multiple locations to support decision making and treat planning, especially in specialties like radiology and oncology.
AI is revolutionizing diagnostics and surgery, what this means for providers and patients, and how healthcare organizations can responsibly adopt these tools for their digital transformation. We’ll look at both the opportunities and the challenges, including safety, reliability, data privacy, and trust.

Generative AI has evolved from a buzzword to a backbone of modern healthcare. These advanced algorithms don’t just analyze existing data, they can generate text, images, and even synthetic medical records to support doctors, nurses, and administrators. In 2025, generative models help create individualized care plans, summarize patient histories, and simulate rare disease scenarios to improve training and response.
The scalability of generative AI is crucial for healthcare systems facing clinician shortages and rising patient expectations. By automating repetitive documentation and synthesizing vast datasets, AI enables providers to focus their expertise where it matters most: on patient care. Hospitals using these technologies report significant time savings and improved job satisfaction among staff.
For healthcare leaders, embracing generative AI is not only about adopting tools, it’s about reimagining workflows and redefining the role of clinicians in a digital-first era. Those who lead this change are setting new standards for operational efficiency and clinical excellence.
Virtual assistants in healthcare have evolved far beyond basic chatbots. Today’s AI-powered assistants can schedule appointments, answer clinical questions, and guide patients through any moment of healthcare using natural language understanding. They are prepared in EHR platforms, mobile apps, and even hospital kiosks, providing always-on support to both patients and staff.
A standout example is the use of AI assistants for patient check-in and first evaluation. By collecting patient symptoms and medical history in real time, these systems help route cases to the right specialists, flag urgent concerns, and reduce bottlenecks in emergency departments. The result is a smoother, faster, and more personalized patient journey.
For clinicians, virtual assistants can summarize long patient notes, highlight medication conflicts, and surface key trends from the EHR. This not only saves time but also reduces cognitive overload, making it easier to focus on complex decision-making and direct patient interaction.
Diagnostics is one of the most promising frontiers for generative AI. In radiology, pathology, and genomics, AI models now assist in analyzing complex images, identifying subtle anomalies, and even predicting disease risk before symptoms appear. Philips’ 2025 trends highlight the widespread adoption of AI-powered diagnostic platforms in leading hospitals worldwide.
These tools augment the capabilities of human experts, catching patterns that might be missed due to fatigue or cognitive bias. In breast cancer screening, for instance, AI models have demonstrated higher accuracy in detecting early-stage tumors, leading to improved outcomes and reduced false positives. Similar advances are being seen in cardiology, dermatology, and ophthalmology.
Crucially, AI-driven diagnostics also help democratize access to specialist expertise. Rural or under-resourced clinics can leverage cloud-based AI tools to interpret scans or lab results, narrowing gaps in healthcare equity and ensuring patients receive timely, accurate diagnoses wherever they are.
Clinical documentation is a major source of burnout for healthcare professionals, consuming hours each day that could be spent on patient care. Generative AI is changing this paradigm by automatically transcribing, summarizing, and structuring clinical notes. Virtual scribes listen to doctor-patient interactions and generate accurate, context-aware summaries for the EHR.
This technology doesn’t just speed up note-taking, it ensures consistency, improves billing accuracy, and enables richer data for research and population health management. AI-powered summarization tools can highlight key symptoms, risk factors, and follow-up needs, reducing the risk of missed details or miscommunication.
Leading hospitals report that implementing generative AI for documentation decreases after-hours work for physicians, boosts job satisfaction, and even shortens patient wait times. As these tools continue to evolve, they will become a standard part of the clinical toolkit, freeing up more time for human connection.
Perhaps the most exciting application of AI in healthcare is in the operating room. AI now plays a role in surgical planning, intraoperative navigation, and even real-time decision support. Surgeons use AI models to simulate different approaches, predict complications, and optimize outcomes for each patient.
Robotic systems, guided by AI, can perform minimally invasive procedures with unmatched precision. These platforms use live imaging and generative models to adjust in real time, compensating for patient movement or unexpected anatomical variations. The result is faster recovery, fewer complications, and greater consistency across surgical teams.
A lot of trends highlight the integration of generative AI in surgical robots that can “learn” from thousands of prior cases, suggesting optimal incision points and tool trajectories. Surgeons remain in control, but the AI acts as a tireless co-pilot, improving safety, outcomes, and patient confidence in the surgical process.

AI for surgery, next step for healthcare. Photo by Pavel Danilyuk on Pexels: https://www.pexels.com/photo/woman-lying-on-a-massage-table-and-getting-treated-by-a-robot-8439072/
Adopting generative AI in healthcare brings significant benefits, but also new challenges. On the positive side, AI reduces administrative burden, decreases diagnostic errors, and delivers faster, more precise care. It helps address workforce shortages and supports clinicians with decision-making and personalized recommendations.
However, pain points remain. Data privacy and security are top concerns, as AI systems require access to sensitive patient information. There are also challenges around bias in training data, explainability of AI decisions, and integration with existing EHR systems. Clinician acceptance is another challenge: some worry about “automation anxiety” or losing their professional autonomy.
To maximize benefits and minimize risks, healthcare organizations must invest in robust governance, transparent AI models, and ongoing staff education. The goal is not to replace humans, but to empower them with smarter, more intuitive tools that make care safer and more effective.
دعنا نبني شيئاً استثنائياً معاً.
اعتمد على شركة Lasting Dynamics للحصول على جودة برمجيات لا مثيل لها.
On the other hand, we also need to mention some of the benefits AI presents to overcome these challenges:
Despite the promise, several challenges persist. Data silos, legacy IT, and lack of skilled personnel can slow down adoption. Resistance to change, whether from rank-and-file clinicians or leadership, remains a common stumbling block. Concerns about liability, accountability, and the risk that must be addressed with clear protocols and human-in-the-loop safeguards.
Budget constraints also play a role. While generative AI can deliver significant long-term savings, upfront investments in infrastructure, training, and integration are substantial. Smaller clinics and under-resourced hospitals may struggle to keep pace without targeted funding or public-private partnerships.
Recognizing and proactively addressing these pain points is essential for a successful AI journey. The path is complex, but the rewards, in better patient outcomes, operational efficiency, and staff satisfaction, are transformative.
For generative AI to deliver on its promise, seamless integration with existing healthcare IT infrastructure is essential. Many hospitals and clinics still operate with siloed data, legacy software, and proprietary systems that complicate adoption. Generative AI tools must be able to pull from and write to EHRs, imaging archives, scheduling platforms, and more.
Leading vendors, including Philips we previously mentioned, are prioritizing open APIs, regulation standards, and secure cloud-based platforms to enable interoperability. This ensures that AI-generated insights are available at the point of care, regardless of where the data originated.
The result is a unified clinical workflow, where doctors can access AI-powered recommendations, documentation, and surgical guidance from within their existing tools. For healthcare providers, this reduces friction, improves adoption rates, and maximizes the return on AI investments.
With great power comes great responsibility. The use of generative AI in diagnostics and surgery raises important ethical questions around data privacy, informed consent, and algorithmic bias. Regulations like HIPAA, GDPR, and new AI-specific guidelines in the world, require healthcare organizations to implement robust safeguards and transparent practices.
Key best practices include encrypting patient data, maintaining audit trails of AI decisions, and regularly validating model performance for accuracy and fairness. Informed consent processes must explain when and how AI is used in care delivery.
Organizations that prioritize ethical AI not only avoid legal pitfalls, they also build trust with patients and clinicians. As generative AI becomes more embedded in healthcare, proactive governance and compliance will be key differentiators for leading providers.
Successful AI adoption depends as much on people as on technology. Clinicians need training, not just on how to use new tools, but on understanding their strengths, limitations, and appropriate use cases (like any new equipment). Hospitals must invest in ongoing education, workshops, and simulation labs where staff can interact with AI-powered systems in a safe environment. In other words, it's vital to train the staff to use properly the AI in the workflow.
Change management is critical. Leaders should involve clinicians early in the design and rollout of AI solutions, gathering feedback and addressing concerns. Transparency about how AI makes decisions, and clear protocols for escalating to human oversight, help build confidence and buy-in.
When clinicians feel empowered rather than replaced by AI, adoption rates soar. The ultimate goal is a collaborative model, where human expertise and machine intelligence work hand in hand to improve patient care.

Generative AI holds special promise for improving health equity worldwide. In regions with limited access to doctors or specialists, cloud-based AI tools can deliver expert-level diagnostics and treatment recommendations. Mobile virtual assistants can guide patients through self-care, medication adherence, and follow-up, even in remote or underserved areas.
AI-driven translation and localization ensure that care advice is culturally and linguistically appropriate. In global health crises, such as pandemics or natural disasters, AI models can rapidly analyze emerging data and help coordinate response efforts.
For NGOs, governments, and international health systems, investing in generative AI is a force multiplier, expanding reach, improving quality, and saving lives across borders.
The healthcare AI landscape is rapidly expanding, with startups and established tech firms alike contributing new solutions. Innovative companies are developing specialized generative models for rare diseases, surgical navigation, and remote monitoring. Strategic partnerships between hospitals, vendors, and research institutions accelerate the pace of innovation and facilitate real-world validation.
Healthcare organizations that embrace an ecosystem mindset, sharing data, expertise, and resources, will be best positioned to navigate the fast-evolving world of generative AI. As AI continues to evolve, so too will the regulatory landscape, reimbursement models, and patient expectations. Healthcare organizations that stay ahead of these trends will shape the future of medicine.
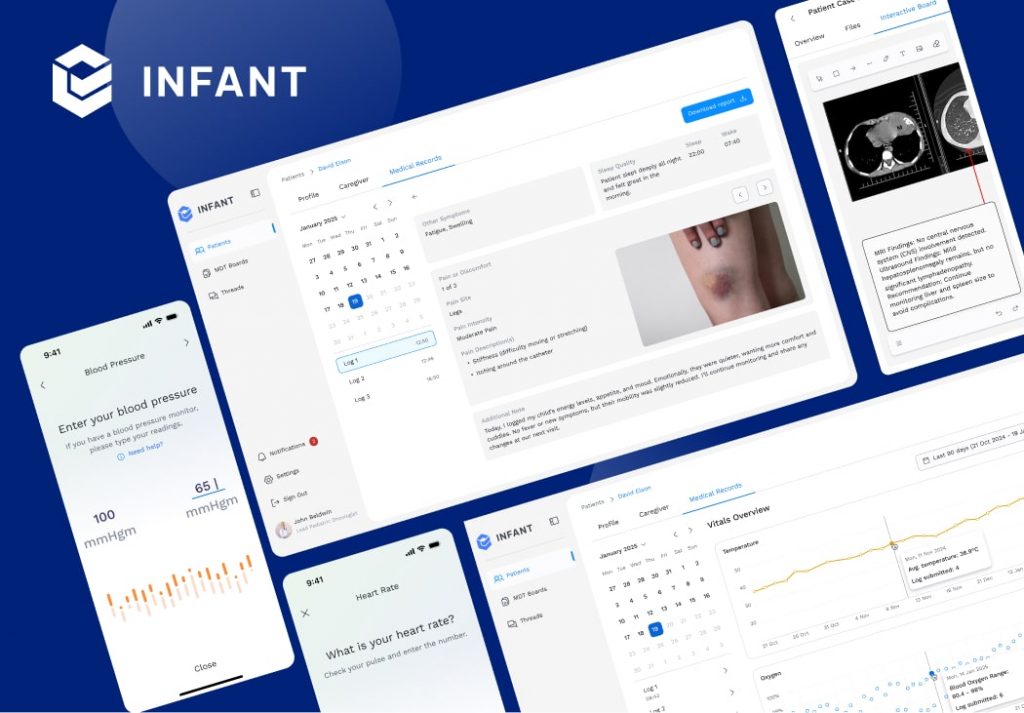
الرضيع is one of Lasting Dynamics’ most innovative healthcare projects, designed to support neonatal care with the help of artificial intelligence. By processing complex medical data in real time, the system assists doctors in monitoring newborns, spotting risks early, and supporting faster, more confident decision-making. Here, AI is not just an assistant, it becomes a safety net for the most fragile patients.
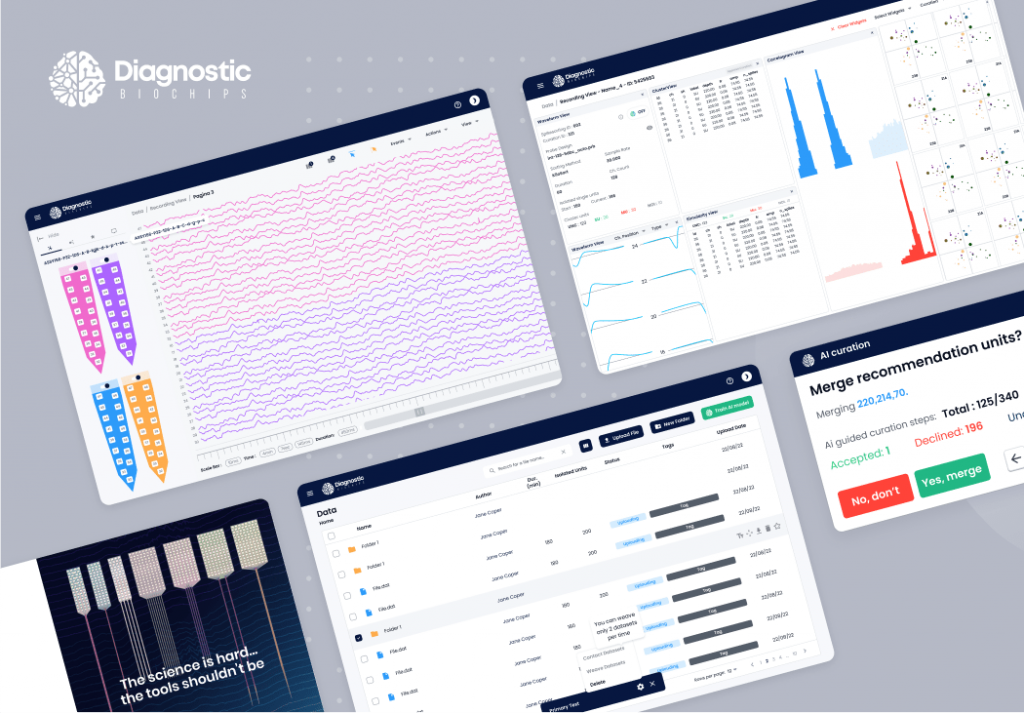
الرقائق البيولوجية التشخيصية (DBC) takes a similar approach, using AI to analyze biological data and uncover patterns that would be impossible to detect manually. This combination of bioengineering and machine learning enables earlier diagnostics and personalized treatment options, giving healthcare providers tools that extend far beyond traditional lab testing.
بدءاً من الفكرة إلى الإطلاق، نقوم بتصميم برامج قابلة للتطوير مصممة خصيصاً لتلبية احتياجات عملك.
شارك معنا لتسريع نموك.
For those interested in seeing how AI extends into other areas, أومني showcases how Lasting Dynamics applies intelligent solutions outside of direct patient care and helps insurance with an engaging app. For more healthcare innovations, visit the healthcare section on the company’s website, or discover the broader client portfolio to see how LD brings the same vision to many industries.
Generative AI has moved from experimental labs to the heart of modern healthcare. From virtual assistants that streamline documentation, to AI-driven diagnostics that catch disease earlier, to surgical robots guided by generative models, the transformation is both profound and accelerating. The benefits, greater efficiency, accuracy, and patient-centered care, are matched by new challenges in privacy, adoption, and equity.
Healthcare leaders and CIOs must act now: investing in integration, staff training, and ethical governance. The future belongs to those who can harness AI’s power to augment, not replace, the human touch. With the right strategy and partners, the surgical revolution is just beginning, and every patient, clinician, and organization can be part of the change.
Ready to experience the power of generative AI for diagnostics and surgery? 👉 للتواصل مع Lasting Dynamics to discover how we can help your healthcare organization lead the next wave of التحوّل الرقمي, delivering safer, smarter, and more human-centered care.
Generative AI models analyze medical images, synthesize patient data, and assist clinicians in identifying diseases earlier and more accurately, improving patient outcomes[[Philips+1]].
Yes, AI-driven robotic systems use live imaging and generative models to assist surgeons in planning and executing procedures with greater precision and flexibility.
Key risks include data privacy breaches, algorithmic bias, lack of explainability, and integration challenges with legacy systems. Robust governance and staff training are essential to mitigate these.
By following data privacy regulations (like HIPAA, GDPR), maintaining clear audit trails, involving clinicians in AI oversight, and regularly testing models for fairness and accuracy.
Benefits include reduced documentation time, higher diagnostic accuracy, improved surgical outcomes, increased staff satisfaction, and better patient engagement.
حوّل الأفكار الجريئة إلى تطبيقات قوية.
Let’s create software that makes an impact together.
لويس لامبرت
أنا مصمم وسائط متعددة ومؤلف إعلانات ومحترف تسويق. أبحث بنشاط عن تحديات جديدة لتحدي مهاراتي والنمو مهنياً.